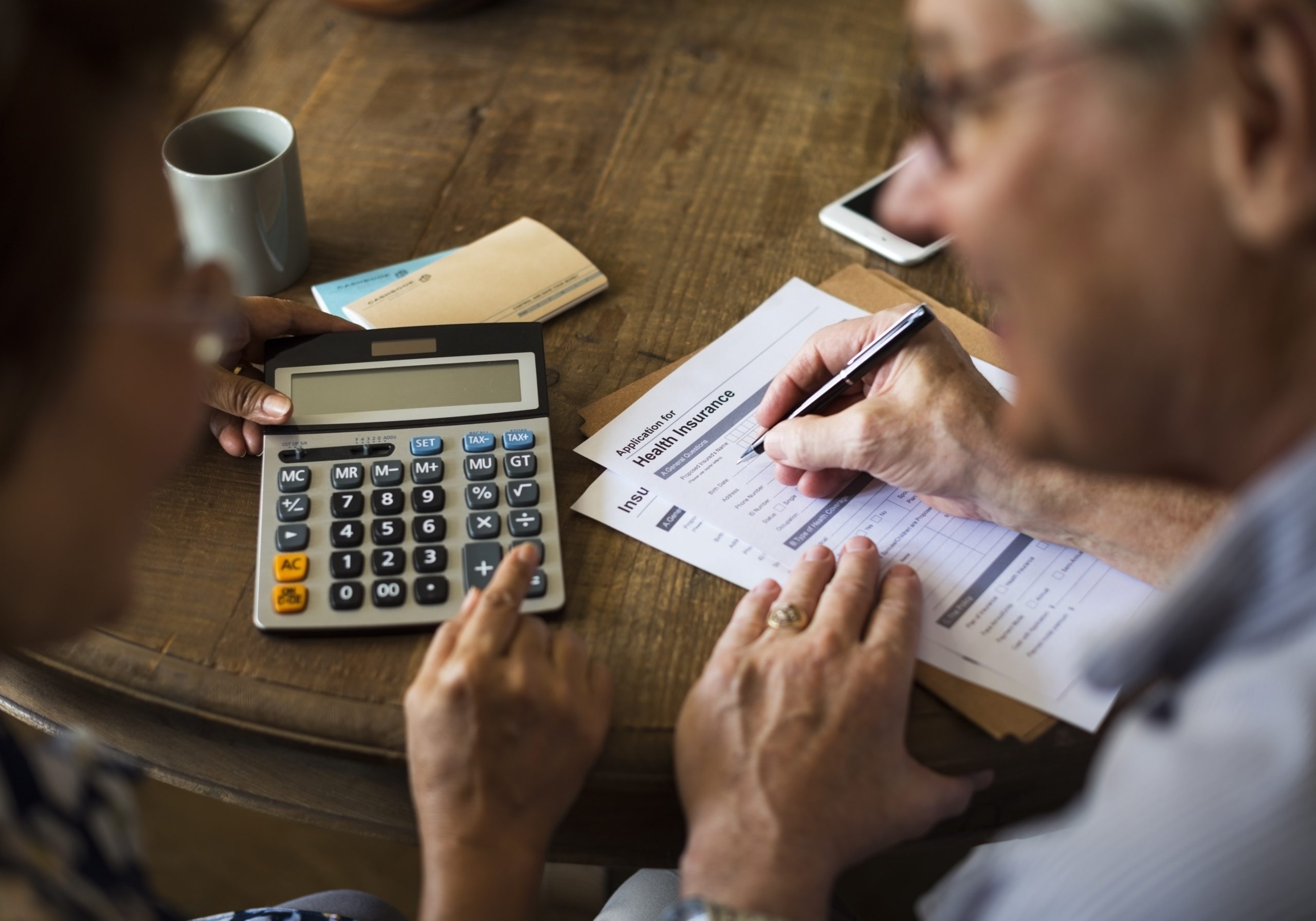
Before you give up on hiring a home care worker, there are resources available to assist you financially. Before we get started, it’s important to recognize that due to economic shifts beyond our control, such as the financial meltdown of 2008, it’s quite possible that despite long-term planning and having done everything right, you can still wind up under-funded for your retirement and health and home care expenses. However, being able to hire a home-care worker is not necessarily out of reach. There are options available to assist you.
With 70 million baby boomers at or reaching retirement age, it’s not unreasonable to expect healthcare costs to increase as insurance companies see a boost to their bottom line. There are insurance policies that cover home care benefits, which can either take the form of long-term care insurance or a life insurance policy with a rider for long-term care. The question is whether you can afford such insurance policies.
According to Genworth’s LTC calculator (California only), the rates for a 60-year old couple calculated at $150 a day, which is that cap for four years, the combined yearly premium is $3476.56, or $289.74 a month, and that’s just an estimate. There is also a 90-day elimination period. Another thing to factor in, if you’re trying to plan ahead, is that one in five applicants below the age of 60 are declined and that ratio rises with age
Those without long-term care insurance often start out relying on an unpaid family caregiver, but eventually many need to turn to paid help. And that can be expensive as well, but there are ways to supplement costs, which we’ll discuss momentarily.
Paying out of pocket
For the most part, those who have home care pay out of their own pocket. Many cobble together a care budget from various sources, including annuities,
investments and savings, and life insurance policies that can be used for qualified home-care expenses through cash value or an accelerated death benefit.
Other sources including borrowing, for example by taking out a reverse mortgage or home equity loan. This is something that you should avoid and keep only as the last resort of last resorts. There are those who believe that they have the right to take what they want by any aggressive means necessary and your home should not be one of those things. Also, from a practical standpoint, using your house to provide cash for long-term care is risky. You could run out of equity in your home while you still need the care.
If you find that you are out of alternatives, research reverse mortgages available only to those 62 and older to see if they are the right solution. The first step in qualifying for a federally approved reverse mortgage is an educational session with a qualified counselor who will guide you through the process and list of fees.
Government help
If you don’t have long-term care insurance and don’t have the financial resources, you can get help paying for in-home care. Start by searching the federal government’s Eldercare Locator to find your local Area Agency on Aging.
These offices are the first place to look since they have resources on home health care and they are the gateway to Medicaid, which pays for home services. You can also check the National Council on Aging’s BenefitsCheckUp to find out what programs you may qualify for.
Help with home-care bills may be available through Medicaid if you have low income or limited assets. Medicare can also pay for home health services in some circumstances. If you are a former service member, the Department of Veterans Affairs (VA) offers home-care support. Additionally, those who pay for caregiving also can qualify for tax breaks.
Medicare
Original Medicare will cover routine home care, which includes help with daily activities such as bathing and dressing and basic medical care such as checking vital signs and dressing wounds. However, only on a part-time or intermittent basis and only if a doctor orders it as part of a broader plan of care. It will not pay for full-time home care or for personal and homemaker services if that is the only help you need.
However, Medicare Advantage (MA) plans, which are private insurance policies that match original Medicare coverage but can provide additional benefits, have the option to offer broader and longer-term coverage for home health services. For example, an MA plan might cover a personal care aide even if the recipient does not need therapy or skilled nursing. If your loved one has MA, check with the plan provider.
Medicaid
The joint federal-state program does pay for in-home care, some residential and assisted living care, and nursing home care. More than half of all Medicaid spending on long-term care goes toward home- and community-based services.
Home health services are less limited under Medicaid than with Medicare, but each state runs its Medicaid program differently, and eligibility and benefits vary.
Veterans’ programs
Eligible former service members may qualify for one of several VA programs that help pay for care at home, including aid and attendance benefits, Housebound benefits, veteran directed are, and homemaker and home health aide care. Contact your regional VA benefits office for information.
Taxes
An adult child serving as a caregiver for a live-in parent may get a tax break by claiming the parent as a dependent. However, certain criteria must be met, including providing more than half of the care recipient’s financial support.
A lesser-known option: PACE
Programs of All-Inclusive Care for the Elderly (PACE) is a small but growing Medicare and Medicaid initiative aimed at keeping frail seniors out of nursing homes. About 45,000 people were enrolled as of May 2019 through more than 100 organizations offering PACE programs in 31 states.
Among other things, PACE covers in-home care, adult daycare, checkups, hospital and nursing home stays, prescriptions and some transportation for medical purposes. It can also pay for training, support and respite for family caregivers.
Local PACE organizations work with medical providers who form the recipient’s health care team. If the team decides your loved one needs care that Medicaid or Medicare doesn’t provide, PACE still may cover it.
People with Medicare, Medicaid or both can qualify, although if you have Medicare only you might be charged a monthly premium. Those not covered through either program can pay for PACE privately.
To be eligible for PACE you must be:
• 55 or older
• In need of nursing home-level care as certified through your state
• A resident of an area with a PACE organization
• Able to live safely in the community with help from PACE.
The PACE program becomes the sole source of services for Medicare and Medicaid eligible enrollees. Individuals can leave the program at any time.
For more information concerning your specific needs and qualifications, contact New Wave Home Care for assistance.